Q&A
Emotion Regulation and Inflammation
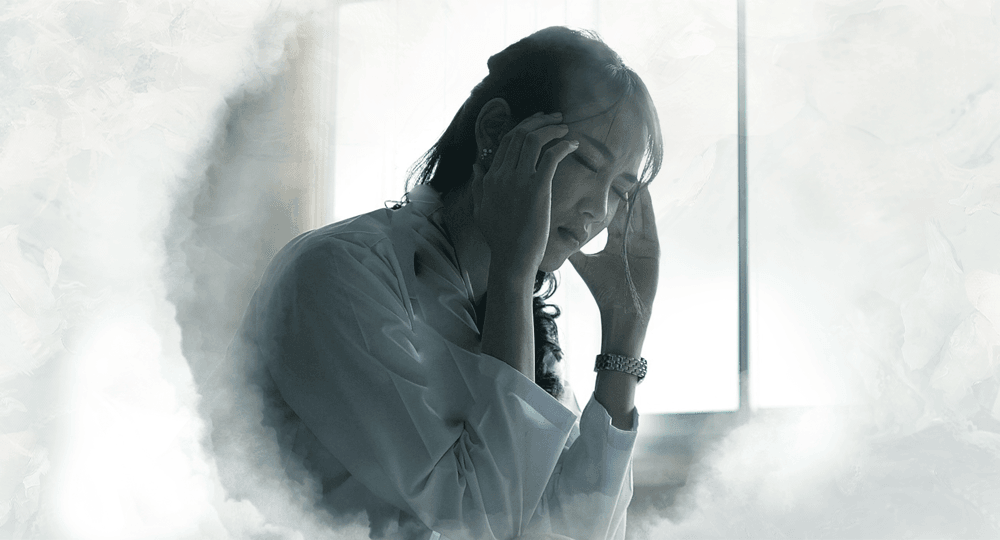
Dr Daniel Moriarity’s groundbreaking research explores the biological links between inflammation and emotion regulation characteristics. This Q&A looks to opportunities for testing and treatment.
Q
What sparked your interest in studying emotion regulation and inflammation?
A
Q
What is the association between emotion regulation and inflammation? Is there potentially a causal relationship?
A
Q
Can inflammatory biomarkers be used for screening and early intervention of disorders associated with emotional dysregulation (for example, ADHD, BPD, and ASD)?
A
Q
Are there specific tests you can suggest for measuring inflammation and emotion regulation?
A
Q
What emotion regulation strategies are associated with vulnerability or resilience to inflammation?
A
Q
Can you recommend any evidence-based practices therapists can use with clients to modulate inflammation?
A
Q
Are inflammatory biomarkers involved in the mechanisms of action for existing interventions, such as antidepressants, mindfulness, and exercise?
A
Q
Is there any research on the use of anti-inflammatory medications in the treatment of disorders associated with emotional dysregulation?
A
Q
Can you touch on the difference between acute and chronic inflammation, and their potential roles in emotion regulation?
A
Q
Are there any projects that you are excited about within the field of precision psychiatry?
A
You may also like