Q&A
Cultural Variables within CBT
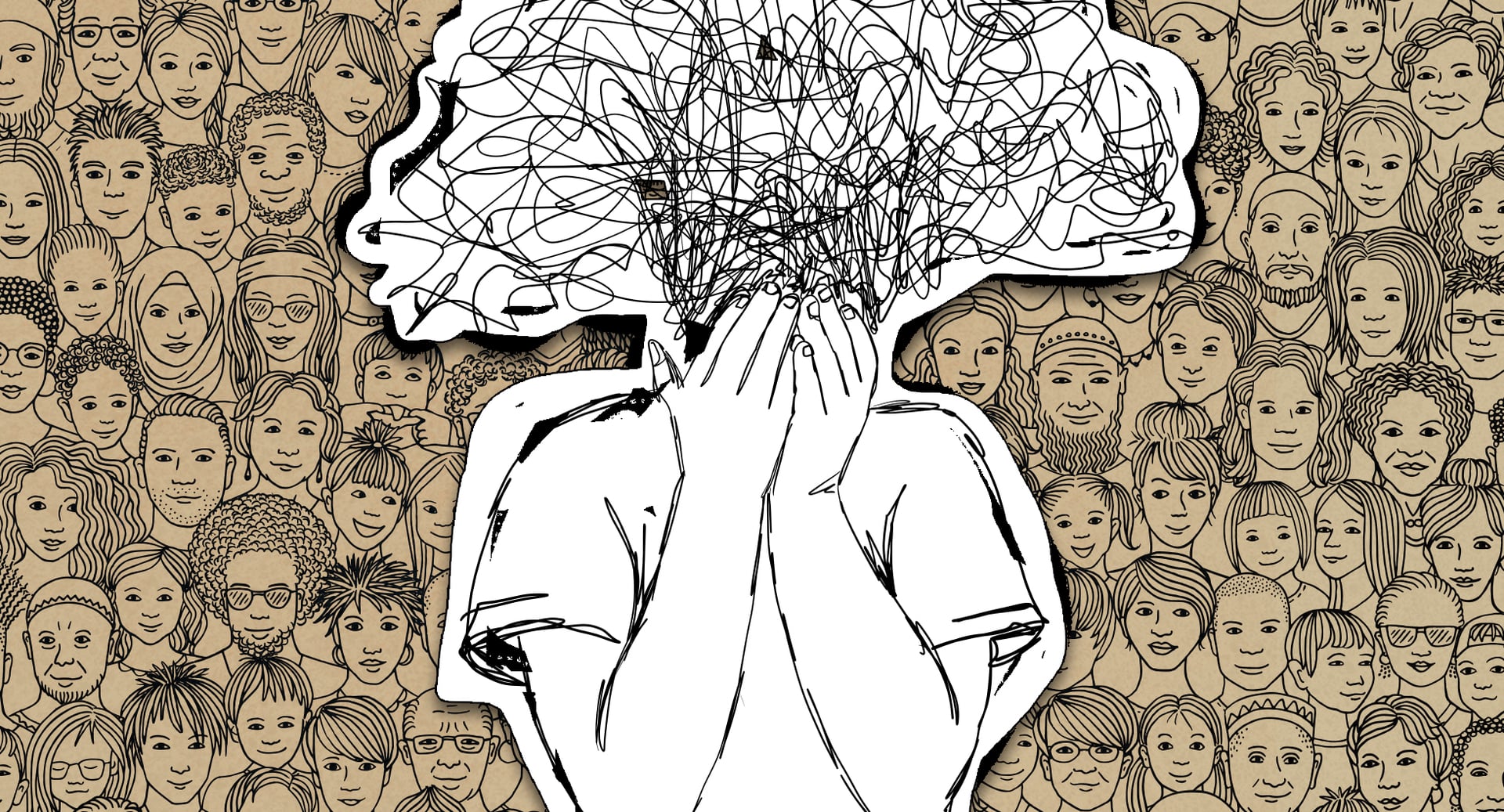
World-leading CBT expert and performance mentor Kevin Chapman answers questions on the importance of cultural awareness when treating clients.
Q
Can you give an example of how anxiety can look or present differently depending on someone's racial or ethnic background?
A pdf
pdf pdf
pdf pdf
pdf
 pdf
pdfWilliams_CrossCulturalOCD_2017
 pdf
pdfChapman_SAD-1_2013
 pdf
pdfChapman_SAD-2_2013
Q
Is it advisable for clients to seek out therapists who have a similar racial identity as they do?
A
Q
I am aware that a key part of treatment for anxiety is learning safety but that this can be hard for people who experience a pervasive sense of unsafety based on their race or identity. Can you give me a brief outline of what anti-racist CBT looks like and how I can be more aware?
A
Q
I work with Asian Americans in NYC where anti-Asian violence has been increasingly rampant. I myself am Asian and also have anxieties about going outside. How can I address this with my clients who are limiting their lives as a result?
A
Q
How can I make culturally sensitive adaptations to CBT for youth in marginal communities with social anxiety disorder? Thanks
A pdf
pdf pdf
pdf
 pdf
pdfChapman_SAD-1_2013
 pdf
pdfChapman_SAD-2_2013
You may also like