Depression and Heart Health
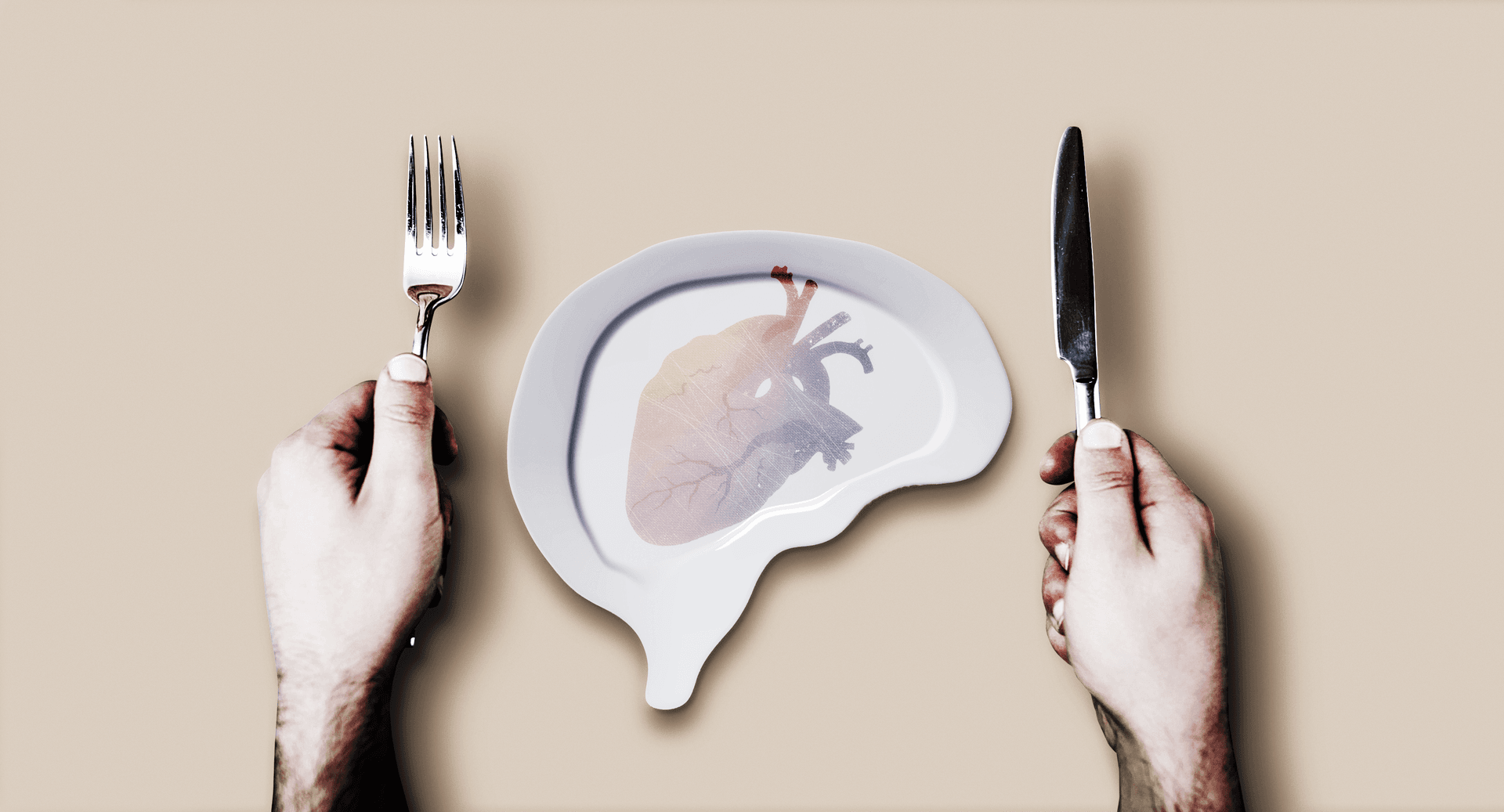
What is the correlation between heart problems and depression, and vice-versa? Behavioral scientist Adrienne O'Neil unravels the research.
One of the key pathways that links the heart and mind is called the vagus nerve. This is a part of the nervous system responsible for many things including our fight or flight response. The vagus nerve counters our physiological reaction (e.g racing heart, sweaty palms) to a threat or stress in a way that strikes a balance so we can respond in a way that is helpful not a hindrance. It has been proposed that people with depression, anxiety and/or distress may not be as efficient at countering that response required to achieve that balance when compared to those without. Over time this may put pressure on the heart and other organs. I am not a medical doctor so cannot advise on your specific circumstances but I would suggest discussing this with your physician as managing mental health should be a key part of managing heart problems because they are so closely linked.
It is really complicated! On face value, one might think that it is due to symptoms of depression (as an example) resulting in people drinking, smoking or eating more/worse and being less active, adherent with medication or socially engaged. All of these things can contribute to heart problems. However even when you account for these factors they still seem to be closely linked. From a biological point of view, heart and mental health conditions actually share some physiological pathways (including the vagus nerve discussed in a previous question). For example, both are inflammatory conditions. This means that both are characterised by the body being in a constant state of low grade inflammation which perpetually incites an immune response. Because of this, it is thought that if we treat one condition, the other will improve but we don't have very good data on what such approaches might be.
One of the million dollar questions! I tend to view this from a lifecourse perspective. The data tell us that depression and anxiety most commonly occur before the age of 25 while most (not all) heart disease manifests in later life. That is not to say however that the beginnings of both diseases don't occur early; it might just be that they present in a clinically meaningful way later on. For example, there is evidence that psychiatric and vascular disorders can develop in the womb! Its called the early life programming hypothesis. Of course, depression can also come about in later life AFTER a heart attack or stroke. So it is certainly bi-directional but many people who have both conditions will have had a history of depression/anxiety first. The only way to really disentangle this is to demonstrate that treating one condition prevents the other. There have been few studies that have looked at this as they are very difficult to do and need to be conducted in a very large group of patients over a very long period.
It is incredibly difficult to separate and identify one! We know that improving different behaviours around lifestyle can have benefits that interact - the total effect is greater than the sum of its parts! But what is also very clear is that lifestyle -which is often viewed as a series of individuals behaviours or choices - does not occur in a vacuum and it heavily influenced by environment, household, neighbourhood, education, income and employment. Improving these "upstream" determinants of health would be incredibly beneficial in shaping individual behaviour and thereby their heart and mental health risk.
I have been involved in co-developing interventions that target all of these lifestyle behaviours (exercise, diet, medication adherence, sleep, smoking and alcohol reduction) as well as those that focus on one behaviour, named dietary improvement. For reasons I mentioned in the previous response, the good thing about multi-component interventions is that the effects can be multiplicative. On the other hand, some patients like to focus on one lifestyle behaviour so it is more achievable than being overwhelmed with many targets; they can master one rather than 5!
Just as mental and heart health share common physiology, they share risk factors and in many cases management strategies. Diet is one of these as it can have pro-inflammatory and anti-inflammatory properties. It is much more well accepted that diet has an influence over physical illness like heart disease and diabetes but its taken much longer for the evidence to be generated for mental health. In 2012, we conducted the first trial in the world to demonstrate that a Mediterranean style diet adjunctive to standard care (meaning, they could still take their medication or therapy) could reduce depressive symptoms in those with clinical depression over 12 weeks. This has now been replicated in 3 other trials.
As discussed in a previous response, approximately 75% of depressive cases manifest before the age of 25 years. That is not to say that people cannot experience anxiety or depression in later life. There are periods of ones life during which they are especially vulnerable to mental health issues. For example, in the post-natal period for women or in later life or old age especially during periods of change like the death of a loved one. With heart disease, men tend to experience it earlier (in their 60s) and women about 10 years later. This is because oestrogen is thought to be somewhat protective for women at least up until menopause. There is some evidence to suggest this 10 year gap is narrowing however for reasons largely unknown.
I am getting more immersed in these data in an attempt to disentangle this association. It's well established that substance use is high in those with mental health issues. For some, mental disorders (e.g drug-induced psychoses) can be a result of drug use. For others who have either a predisposition to or are experiencing mental disorders might use drugs as a coping mechanism, especially individuals who experienced early life trauma. Early life trauma, mental disorders and the associated environments can all contribute to an elevated risk of developing heart disease. It's difficult to know what is driving that association as some would argue that early life conditions are the most potent predictor of both mental and heart disease outcomes. Less is known about the direct relationship between drug use and heart disease. It stands to reason that people with addictions to opioids for example might have elevated risk of sudden cardiac arrest and infective endocarditis (a bacterial infection in the heart). This is something we are currently exploring.
Depression is by far the most commonly studied in relation to heart disease. However some of the first formal studies were conducted in veterans who experienced Post Traumatic Stress Disorder after the war who were found to have elevated risk of heart attack. There is now evidence that anxiety can elevate risk as well as bipolar and schizophrenia however with the latter, there are mediating factors like noxious side effects of medications for example. There is now great interest in identifying sub types of depression and anxiety as it has been hypothesised that somatic and cognitive symptoms may exert differential influence on the cardiovascular system. We are currently exploring this as it will guide treatment strategies, particularly in the post heart attack period.
My personal approach to behavioural medicine is that a non-judgmental approach is required. There is little point in developing efficacious interventions if they fail in their dissemination because they alienate your target population. Of course obesity and overweight is a controversial area. Using diet in the management of depression, our SMILES trial demonstrated that dietary improvement was not dependent on weight loss. In fact over 12 weeks, participants' depression decreased while their weight stayed the same - the dietary program was one of nutritional and caloric adequacy (ie. not calorie restricted). For heart disease, the influence of weight may depend on the condition. In heart failure for example, weight is not a good indicator of outcomes as heavier patients (those with high BMI) tend to live longer but that is likely because those with low BMIs have more frailty and severe disease. There is of course data to show that greater waist circumference and adipose tissue predicts onset of heart disease because (as discuss previously)it is characterised by higher levels of inflammation, amongst other things.
Completing 150 min/week of moderate-vigorous physical activity can be protective against developing both physical condition like heart disease as well as mental health conditions like depression. Even low doses (e.g.< 150 min per week of light-, or moderate-intensity) can reduce risk. It really does depend on the individuals' level of impairment (mental and/or physical; some individuals with heart failure find it difficult to walk around the block). Australian guidelines state that “doing any physical activity is better than doing none”. Mixing up muscle-strengthening and aerobic exercise can reduce depressive symptoms but one doesn't appear superior over the other. Some psychological therapies encourage people to identify activities they enjoy; any activity that is physical that is also enjoyable will likely have added benefits (gardening, playing with grand children, surfing, horse riding, dancing).
In late life depression, MRI studies have shown that vascular lesions lead to depression by disrupting networks called the frontal–subcortical–limbic networks. This is critical for mood regulation. Interestingly, there is some evidence that young adolescents with depression have impaired vascular functioning (arterial stiffness) so again, the relationship appears bidirectional and may well occur earlier than we expect or is clinically evident.
Greater investment in medical research in this area to develop new treatments, early detection and monitor population trends is key. As mentioned in another response, some of the common risk factors for both conditions occur in early life (adversity, poverty, trauma) so investing in early years of life and focussing on the lifecourse is key socio-economic factors like education and employment are critical so the importance of providing a fair safety net for all members of society (universal health care, good minimum wage, policy to protect against homelessness, food accessibility and security, Indigenous Australians, new arrivals and migrants, incarcerated individuals) cannot be understated. It's more difficult to encourage and promote lifestyle behaviours in the absence of these things. There have also been sub populations almost entirely neglected from heart disease research in the past including women (especially pregnant women), Indigenous Australians, new arrivals and migrants and similarly men who have depression (especially elderly men who are at highest risk of suicide). Thus much of the policy and clinical guidelines are based on outdated data or data that is not fully representative of the Australian population.
Older age is one of the strongest risk factors for heart disease. Depression and other mood disorders tend to first occur in early life (before age 25). In fact anxiety commonly occurs anywhere from age 6 years according to US data.
Animal studies suggest that IF slows the accumulation of molecular damage causing cardiometabolic dysfunction that is observed in HF. Rat models showed that IF caused structural changes and improvements in maladaptive remodelling, increased cardiac functioning and improved left ventricular volumes and diameter. In other words, periods without eating (ever seton day) resulted in the generation of new blood vessels. This is the rationale for IF improving both cardiac functioning and mood. One study has been conducted in humans with a type of heart failure called preserved ejection fraction which showed good results for cardiac functioning and quality of life (Published by Kitzman in JAMA) but data are scarce beyond that. It stands to reason that Time Restricted Eating would have the same effects but we need human trials to answer that question. Refer to the work of Dr Sacchin Panda for more info on TRE.
Yes this is perhaps the most popular candidate mechanism and one for which there is the strongest evidence. This is the common pathway by which interventions that are ultimately anti-inflammatory in nature like diet, exercise, stress reduction, some medications, quitting smoking likely exert their influence on both conditions. In addition to lifestyle, we are especially interested in novel anti inflammatory therapies like statins and aspirin on psychiatric conditions for this reason.
Another million dollar question! There have been very few studies that have investigated the impact of treating depression on preventing the onset of a heart event. One that I am aware of is the IMPACT trial (a collaborative care model for managing depression which uses a stepped approach to treatment depending on severity). It showed that depression treatment delivered before the onset of clinical heart disease reduced the risk of a heart event over 8 years. However, a significant reduction was observed for men but not women. This is a common issue in these studies. When depression is treated after a heart attack, it can improve mood and behavioural outcomes and sometimes even risk of having another event but it does not appear to prolong survival. Studies using psychotherapy, SSRI (anti depressants) and combinations of both have not been very successful in improving MACE outcomes (major adverse cardiac events).
Yes as discussed in a previous response, lifestyle factors do explain some but not all of the relationship between the two. Each condition appears to exert an independent influence on the other through shared physiology. The evidence is now strong enough that the America Heart Association has stated that depression is now an independent risk factor for poor outcomes after a cardiac event.
As discussed in another response, there doesn't seem to be evidence of superiority for resistance training over cardio but it is likely that both are required for maximum health benefits. Having said that the guidelines states that any exercise is good exercise. 150min of mod to vig activity appears to have protective effects over depression risk. In addition it seems important to do what is enjoyable. Our team is studying the effects of surfing and mental health for example. For heart disease, it is largely dependent upon on the individual's baseline level and level of cardiac functioning. Supervised exercise is needed in the post-cardiac period (strength and cardio). Bed rest is certainly not best for the patient anymore as was thought in the 1960s but we know now how bad sedentary activity is in driving muscle wastage.
One things that is not clear from our SMILES trial (Mediterranean diet for the management of depression) is that we simply don't know what drove the improvements in depression. We know that adherence to the diet was closely correlated with reductions in depressive symptoms. But whether this was because people cut out junk or whether there was something special about the macro/micronutrient profile of the diet remains unclear as the trial was not big enough to look at this. The diet provided ∼11 MJ of daily energy, and was high in fat (40% of energy; >50% from monounsaturated fats), low to moderate in carbohydrate (36% of energy), moderate in protein (18% of energy), and moderate in alcohol (2% of energy from red wine). It was high in fibre (50 g/d), folate (709 μg/d), and vitamin C (247 mg/d) consistent with large quantities of fruits (411 g/d) and vegetables (709 g/d). It met all Recommended Dietary Intakes (RDI) or Adequate Intake (AI) requirements for adult males and females. There are some animal data from psychiatric conditions like schizophrenia that suggest that elimination diets (eg. keto) may be beneficial. Indeed, it is likely that different people will need personalised dietary approaches based on their clinical profile and symptoms. With respect to cardio-protective diets, Mediterranean style diets have by far the strongest evidence. We have shown that a diet with high levels of pro-inflammatory properties (traditional Western diet) predicts onset of heart disease in Australian men over 5 years. I suspect that in the future, more personalised approaches to dietary interventions will benefit cardiac patients as well as psychiatric patients and indeed the general population as we get more sophisticated with personalised medicine.